MASA : 8.30am -12.00pm
TARIKH : 12 APRIL 2010
TEMPAT : HOSPITAL SULTANAH NUR ZAHIRAH
ini ntah temujanji mak yang keberapa...
mungkin ketiga or keempat...
bangun seawal 6 pagi...
budget nk pergi kul 7pg..
tp lari timing..kul 8pg baru gerak dr umah..
dgn memandu Myvi Family menuju ke HSNZ..
dah sampai daftar diri..terus pergi tingkat 1...
bahagian endoskopi..
emm...agak lama menunggu giliran
walaupun dpt no.2...
n akhirnya sampai jg turn..
(aku tak dibenarkan masuk tuk mengikuti prosedur tu..
hehehe..igt leh la tgk cara2 diorag buat..huhu..)
dan gmbr ini adalah hasil endoskopi...

conclusion doktor mengatakan benda ini jarang terjadi...
dan jarang terdapat kes yang cam ni...
so buat sementara ini dikategorikan sbg Gastric Varices..
so untuk mendapat kepastian samada ini adalah btul tau tak...
temujanji seterusnya akan disusuli ke SOPD (surgery).....
dalam masa 2 minggu lagi dan ujian darah diuji lagi....
samada berkaitan dgn hati atau tidak...
if semua result tu ok n tak de masalah...
ia hanya perkara biasa...tp klu sebaliknya..
susulan akan dibuat....
so dibawah adalah keterangan ttg Gastric Varices..
Gastric Varices (From Wikipedia, the free encyclopedia)
| Gastric Varices |
| Classification and external resources |

Isolated gastric varices of Sarin classification IGV-1 seen on gastroscopy in a patient with
portal hypertension |
Gastric varices are dilated submucosal veins in the stomach, which can be a life-threatening cause of upper gastrointestinal hemorrhage. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins which drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours. Patients with bleeding gastric varices can present with bloody vomiting (hematemesis), dark, tarry stools (melena), or frank rectal bleeding. The bleeding may be brisk, and patients may soon develop shock. Treatment of gastric varices can include injection of the varices with cyanoacrylate glue, or a radiological procedure to decrease the pressure in the portal vein, termed transjugular intrahepatic portosystemic shunt or TIPS. Treatment with intravenous octreotide is also useful to shunt blood flow away from the stomach's circulation. More aggressive treatment including splenectomy (or surgical removal of the spleen) or liver transplantation may be required in some cases.
Clinical presentation
Gastric varices can present in two major ways. First, patients with cirrhosis may be enrolled in screening gastroscopy programs to detect esophageal varices. These evaluations may detect gastric varices that are asymptomatic. When gastric varices are symptomatic, however, they usually present acutely and dramatically with upper GI hemorrhage. The symptoms can include hematemesis, or vomiting blood; melena, passing black, tarry stools; or passing maroon stools or frank blood in the stools. Many patients with bleeding gastric varices present in shock due to the profound loss of blood.
Secondly, patients with acute pancreatitis may present with gastric varices as a complication of thrombosis of the splenic vein. The splenic vein sits over the pancreas anatomically and inflammation or cancers of the pancreas may result in thrombosis, or clotting of the splenic vein. As the short gastric veins of the fundus of the stomach drain into the splenic vein, thrombosis of the splenic vein will result in increased pressure and engorgement of the short veins, leading to varices in the fundus of the stomach.
Laboratory testing usually shows anemia and often thrombocytopenia (a low platelet count). If cirrhosis is present, there may be coagulopathy manifested by a prolonged INR; both of these may worsen the hemorrhage from gastric varices.
In very rare cases, gastric varices are caused by splenic vein occlusion as a result of the mass effect of slow-growing pancreatic neuroendocrine tumors.
Diagnosis and classification
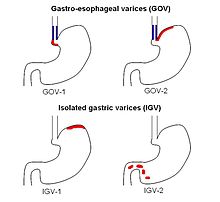
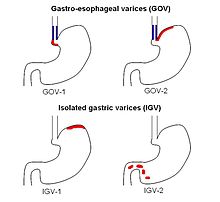
The Sarin classification of gastric varices identifies two types of gastroesophageal varices, where esophageal varices are found concurrently, and two types of isolated gastric varices, found in the absence of esophageal varices.

Antral varices, of Sarin classification IGV-2, an unusual class of gastric varices.
Diagnosis of gastric varices is often made at the time of upper endoscopy.
The Sarin classification of gastric varices identifies four different anatomical types of gastric varices, which differ in terms of treatment modalities.
Treatment
Initial treatment of bleeding from gastric varices focuses on resuscitation, much as with esophageal varices. This includes administration of fluids, blood products, and antibiotics.
The results from the only two randomized trials comparing band ligation vs cyanocarylate suggests that endoscopic injection of cyanoacrylate, known as gastric variceal obliteration or GVO is superior to band ligation in preventing rebleeding rates. Cyanoacrylate, a common component in 'super glue' is often mixed 1:1 with lipiodol to prevent polymerization in the endoscopy delivery optics, and to show on radiographic imaging. GVO is usually performed is specialized therapeutic endoscopy centers. Complications include sepsis, embolization of glue, and obstruction from polymerization in the lumen of the stomach.
Other techniques for refractory bleeding include: